Understanding High Cortisol Levels
What is cortisol and its physiological role?
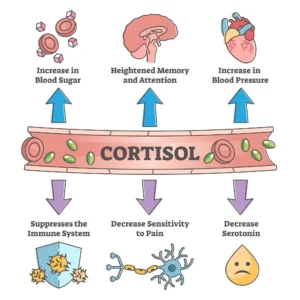
Cortisol is a glucocorticoid hormone produced by the adrenal glands, which are located atop each kidney. This hormone is integral to the body’s stress response, often referred to as the “stress hormone.” It is released into the bloodstream in response to stress and low blood glucose levels. The hypothalamic-pituitary-adrenal (HPA) axis regulates cortisol production, where the hypothalamus releases corticotropin-releasing hormone (CRH), stimulating the pituitary gland to secrete adrenocorticotropic hormone (ACTH). ACTH then prompts the adrenal glands to produce cortisol. This hormone plays a key role in increasing blood glucose through gluconeogenesis, suppressing the immune system, and aiding in metabolism. Cortisol also affects various bodily functions beyond stress response. It influences metabolism by regulating how the body converts proteins, carbohydrates, and fats into energy. This hormone helps control blood pressure, ensuring that the cardiovascular system functions properly. Cortisol’s anti-inflammatory properties reduce inflammation, which is crucial for maintaining homeostasis. Additionally, cortisol affects circadian rhythms, impacting sleep patterns and potentially leading to insomnia if imbalanced. The hormone peaks in the morning, promoting alertness, and gradually decreases throughout the day, preparing the body for rest. Chronic elevation of cortisol levels can lead to significant health issues. High cortisol, often associated with prolonged stress, can result in Cushing’s syndrome, characterized by symptoms like weight gain, particularly around the abdomen and face, and high blood pressure. Excessive cortisol can also cause anxiety and depression, as it affects neurotransmitter systems in the brain. Furthermore, elevated cortisol may contribute to fatigue, as it disrupts normal energy metabolism and sleep cycles. Understanding cortisol’s physiological role is essential for recognizing the importance of maintaining balanced hormone levels to support overall health and well-being. The regulation of cortisol involves a feedback loop to prevent hypercortisolism. When cortisol levels rise, they provide negative feedback to the hypothalamus and pituitary gland, reducing CRH and ACTH release. This mechanism ensures that cortisol production is controlled, preventing the adverse effects of prolonged exposure to high hormone levels. Dysregulation can result in conditions like Cushing’s syndrome or Addison’s disease, where cortisol levels are insufficient. Understanding the multifaceted roles of cortisol underscores the need for balance to avoid health complications such as anxiety, depression, and fatigue.
Why is it important to maintain balanced cortisol levels?
Balanced cortisol levels are crucial for maintaining metabolic health and preventing the negative effects of hormone dysregulation. Elevated cortisol, often due to chronic stress, can lead to metabolic syndrome, characterized by insulin resistance, central obesity, and hypertension. This hormone promotes visceral fat accumulation, contributing to weight gain and increasing the risk of cardiovascular diseases. Prolonged high cortisol levels can also lead to muscle catabolism, reducing muscle mass and strength. Maintaining balanced cortisol helps prevent these metabolic issues and supports overall health. Cortisol balance is vital for immune function. While cortisol’s anti-inflammatory properties help prevent excessive immune responses, chronic elevation can suppress immune function, increasing susceptibility to infections. Cortisol inhibits lymphocyte proliferation and cytokine production, essential for the immune response. However, maintaining cortisol within physiological limits is crucial to avoid compromising the body’s defense mechanisms. This balance is particularly important for preventing fatigue and ensuring the body’s resilience against stress and illness. Mental health is significantly impacted by cortisol levels. Cortisol receptors are abundant in brain regions involved in mood regulation, such as the hippocampus and prefrontal cortex. Chronic high cortisol levels can lead to hippocampal atrophy, impairing memory and learning. They can also exacerbate mood disorders like depression and anxiety by altering neurotransmitter systems. Conversely, insufficient cortisol can result in fatigue and cognitive deficits. Ensuring balanced cortisol levels supports emotional resilience and cognitive function, reducing the risk of anxiety and depression. Balanced cortisol levels are essential for cardiovascular health. Cortisol influences blood pressure regulation through its effects on vascular tone and sodium retention. Chronic hypercortisolism can lead to hypertension, increasing cardiovascular risk and contributing to heart disease. Conversely, low cortisol levels can cause hypotension. Maintaining cortisol within an optimal range is crucial for cardiovascular stability and reducing the risk of conditions like Cushing’s syndrome. Understanding the implications of cortisol balance highlights its critical role in health maintenance, preventing issues such as weight gain, insomnia, and fatigue.
Recognizing Symptoms of High Cortisol
What are the most common symptoms of high cortisol?
High cortisol levels, often linked to chronic stress and adrenal gland dysfunction, present a range of symptoms that significantly affect health. A primary symptom is weight gain, particularly around the abdomen and face, due to cortisol’s influence on metabolism and fat distribution. This weight gain is often accompanied by increased appetite and cravings for high-calorie foods, exacerbating obesity. Muscle weakness and fatigue are also common, as cortisol leads to muscle protein breakdown, reducing physical strength and endurance. This fatigue can be debilitating, affecting daily activities and overall quality of life. Psychological symptoms associated with high cortisol include anxiety and depression. Cortisol affects neurotransmitter balance, impacting mood regulation and leading to heightened anxiety and depressive symptoms. Insomnia and poor sleep quality are also prevalent, as cortisol disrupts the sleep-wake cycle. This creates a cycle where lack of sleep further elevates cortisol, worsening both physical and mental health. Cognitive impairments, such as difficulty concentrating and memory lapses, are also linked to high cortisol, affecting mental clarity and decision-making. High cortisol significantly impacts cardiovascular health, leading to increased blood pressure and heart rate. This raises the risk of hypertension and cardiovascular disease over time. Headaches or migraines may also occur due to these changes. Cortisol’s effect on blood sugar regulation can result in hyperglycemia, increasing the risk of type 2 diabetes. In some cases, high cortisol levels suppress the immune system, making individuals more susceptible to infections and reducing wound healing efficiency. These symptoms are often seen in conditions like Cushing’s syndrome, where cortisol levels are chronically elevated.
How do symptoms vary between men and women?
The symptoms of high cortisol can manifest differently in men and women due to hormonal variations. In women, high cortisol levels can disrupt menstrual cycles, causing irregular periods or amenorrhea. This occurs because cortisol interferes with the hormones estrogen and progesterone, essential for reproductive health. Women may also experience worsened premenstrual syndrome (PMS) symptoms, such as mood swings and bloating, as cortisol exacerbates hormonal fluctuations. High cortisol can also contribute to polycystic ovary syndrome (PCOS), characterized by irregular periods and ovarian cysts. In men, high cortisol levels can lead to decreased testosterone production, resulting in symptoms like reduced libido, erectile dysfunction, and decreased muscle mass. Cortisol’s suppression of testosterone can also cause mood disturbances, including irritability, anxiety, and depression. Men may experience a loss of energy and motivation, affecting both personal and professional life. Additionally, high cortisol can lead to increased visceral fat accumulation, associated with a higher risk of metabolic disorders and cardiovascular disease. Both men and women may experience skin changes due to high cortisol levels. Cortisol increases oil production, leading to acne breakouts and other skin issues. Hair thinning or loss is another common symptom, as cortisol disrupts the hair growth cycle. Cortisol’s impact on bone density can lead to an increased risk of osteoporosis, particularly in postmenopausal women already at higher risk for bone loss. Understanding these gender-specific variations in symptoms can aid in the diagnosis and management of high cortisol levels, ensuring effective treatment approaches tailored to individual needs.
When should one consult a healthcare professional?
Consulting a healthcare professional is crucial when symptoms of elevated cortisol, such as chronic fatigue, weight gain, and insomnia, persist. These symptoms may indicate an imbalance in the hormone cortisol, often linked to stress or adrenal dysfunction. If these symptoms are accompanied by high blood pressure or anxiety, it becomes even more imperative to seek medical advice. A healthcare provider can perform diagnostic tests to evaluate cortisol levels and assess the function of the adrenal glands, providing insights into potential underlying conditions like Cushing’s syndrome. Individuals with a family history of endocrine disorders should be vigilant. Conditions such as Cushing’s syndrome can lead to excessive cortisol production, resulting in symptoms like weight gain and depression. If there is suspicion of such disorders, early consultation with an endocrinologist is advisable. They can recommend comprehensive evaluations, including hormone assays and imaging studies, to determine if the adrenal glands are contributing to the elevated cortisol levels. Timely intervention can prevent complications and improve overall health outcomes. Those managing chronic illnesses exacerbated by high cortisol, such as diabetes or hypertension, should maintain regular healthcare consultations. Elevated cortisol can worsen these conditions, necessitating adjustments in treatment plans. For example, corticosteroid medications prescribed for inflammation can increase cortisol levels. A healthcare professional can guide on medication management to balance cortisol production. Regular monitoring through blood tests ensures the adrenal glands are functioning optimally, reducing the risk of complications associated with prolonged hormone imbalance. If stress management techniques fail to alleviate symptoms like anxiety or fatigue, professional intervention may be necessary. Persistent stress can lead to chronic activation of the HPA axis, elevating cortisol levels. Healthcare providers can offer specialized interventions, such as cognitive-behavioral therapy or pharmacotherapy, to address stress effectively. Managing stress is critical in regulating cortisol and preventing long-term health issues. Consulting a healthcare professional ensures access to a range of therapeutic options tailored to individual needs, helping to stabilize hormone levels and improve well-being.
Underlying Causes of Elevated Cortisol
What are the primary causes of increased cortisol production?
The body’s response to stress is a primary cause of increased cortisol production. Stress triggers the hypothalamic-pituitary-adrenal (HPA) axis, leading to cortisol secretion. While essential for immediate stress responses, chronic stress results in sustained hormone release. Factors such as demanding work environments, financial pressures, and interpersonal conflicts contribute to this chronic activation. Techniques like mindfulness and lifestyle modifications can mitigate stress and help regulate hormone levels, reducing the risk of fatigue and anxiety. Medical conditions significantly influence cortisol production. Cushing’s syndrome, characterized by excessive cortisol, often results from adrenal or pituitary tumors. These conditions disrupt normal hormone regulation, necessitating medical intervention. Other disorders, like polycystic ovary syndrome (PCOS) or thyroid imbalances, can also alter cortisol metabolism. Comprehensive diagnostic evaluations, including blood tests and imaging, are essential to identify these causes. Addressing these medical conditions is crucial for restoring hormone balance and preventing complications such as weight gain and high blood pressure. Psychiatric disorders are linked to dysregulated cortisol production. Depression and anxiety disorders often involve chronic stress responses, leading to elevated cortisol. These conditions require targeted treatment strategies. Pharmacotherapy, including antidepressants, can help manage neurotransmitter imbalances, while psychotherapy provides coping mechanisms for stress. Addressing the psychiatric component is vital for cortisol regulation, as untreated mental health issues can exacerbate hormone imbalances and lead to symptoms like insomnia and fatigue. Lifestyle factors play a significant role in cortisol production. Poor sleep quality or sleep deprivation disrupts circadian rhythms, affecting cortisol release. Dietary habits, such as high sugar intake, stimulate cortisol secretion. Physical inactivity or excessive exercise without recovery can also impact hormone balance. Addressing these lifestyle factors through improved sleep hygiene, balanced nutrition, and regular exercise helps regulate cortisol levels. A holistic approach, combining medical and lifestyle interventions, is often necessary to achieve optimal hormone regulation and prevent associated health complications.
How do external factors contribute to cortisol imbalance?
External factors significantly contribute to cortisol imbalance, affecting the stress hormone regulation within the body. Psychological stressors, such as work-related pressure, personal conflicts, and financial difficulties, can elevate cortisol levels, leading to adrenal fatigue. Chronic stress activates the hypothalamic-pituitary-adrenal (HPA) axis, resulting in prolonged cortisol production. This persistent activation can disrupt the body’s ability to maintain hormonal balance, increasing the risk of anxiety and depression. The continuous stress response can lead to insomnia, further exacerbating cortisol imbalance and contributing to overall fatigue. Environmental factors, including noise pollution, light exposure, and temperature extremes, also impact cortisol levels. Noise pollution in urban areas can induce stress, triggering the release of the stress hormone. Exposure to artificial light, especially at night, disrupts circadian rhythms, affecting cortisol secretion and leading to insomnia. This disruption can cause irregular sleep patterns, contributing to adrenal fatigue and weight gain. Temperature extremes act as stressors, prompting the adrenal glands to produce more cortisol as an adaptive response, which can further imbalance the hormone levels. Dietary habits and lifestyle choices are crucial external factors influencing cortisol balance. A diet high in processed foods, sugar, and caffeine can stimulate cortisol production, while nutrient deficiencies impair the body’s ability to regulate this hormone. Essential nutrients like vitamin C, magnesium, and omega-3 fatty acids are vital for cortisol metabolism and stress response. Physical activity levels play a role; moderate exercise helps regulate cortisol, but excessive or insufficient activity can lead to imbalances. Overtraining results in chronically elevated cortisol, contributing to weight gain, while a sedentary lifestyle can lead to higher baseline cortisol levels, promoting anxiety and stress. Social and cultural factors further influence cortisol regulation. Positive social interactions and strong support networks can buffer against stress, reducing cortisol production. Conversely, social isolation, discrimination, or lack of support can increase cortisol levels, contributing to anxiety and depression. Cultural norms and expectations can impact stress levels and cortisol production, as individuals may experience stress related to societal pressures or cultural identity. Effective stress management strategies are crucial for maintaining hormonal balance, as individuals who perceive stress as overwhelming may experience greater cortisol dysregulation, leading to adrenal fatigue.
Health Risks Associated with High Cortisol
Sustained high cortisol levels pose significant health risks, particularly affecting metabolic and cardiovascular systems. Elevated cortisol is closely linked to insulin resistance, increasing the risk of type 2 diabetes. The stress hormone promotes gluconeogenesis, raising blood glucose levels and impairing insulin sensitivity. This metabolic disturbance contributes to weight gain, especially visceral fat accumulation, associated with metabolic syndrome. Dyslipidemia, characterized by elevated triglycerides and low-density lipoprotein (LDL) cholesterol, is another consequence of high cortisol, further increasing cardiovascular risk. The cardiovascular system is vulnerable to chronic high cortisol, leading to hypertension and increased blood pressure. Elevated cortisol levels can cause sodium retention and vascular resistance, contributing to atherosclerosis. This condition involves plaque buildup in arterial walls, narrowing arteries and restricting blood flow, increasing the risk of heart attack and stroke. Cortisol affects the heart by increasing cardiac output and heart rate, straining the cardiovascular system. Additionally, cortisol promotes inflammation, a key factor in cardiovascular diseases, as chronic inflammation damages blood vessels and exacerbates plaque formation. Mental health is significantly impacted by high cortisol levels. The stress hormone affects mood and cognitive function, with chronic elevation linked to anxiety and depression. High cortisol levels alter neurotransmitter function and brain structure, impairing neurogenesis and synaptic plasticity. This is particularly evident in the hippocampus and prefrontal cortex, areas involved in memory and emotional regulation. Over time, these changes result in learning and memory difficulties, increased susceptibility to mood disorders, and overall mental health decline, further contributing to insomnia and stress. The immune system is adversely affected by high cortisol levels due to the hormone’s immunosuppressive effects. Prolonged cortisol elevation increases susceptibility to infections and slows wound healing, altering immune cell function and reducing the body’s ability to mount an effective immune response. Chronic high cortisol can also increase the risk of autoimmune diseases, as dysregulation of immune function results in the body attacking its own tissues. This immunosuppressive effect, combined with the pro-inflammatory state induced by cortisol, leads to complex immune responses compromising health. Additionally, conditions like Cushing’s syndrome can develop, characterized by prolonged exposure to high cortisol levels, further increasing health risks.
What are the potential long-term health impacts?
The long-term health impacts of sustained high cortisol levels are extensive, affecting various physiological systems. One significant consequence is adrenal fatigue, where chronic cortisol elevation overworks the adrenal glands, leading to inadequate hormone production. Symptoms include fatigue, muscle weakness, and diminished stress response. Over time, this can progress to adrenal insufficiency, where the body cannot effectively cope with stress, resulting in severe health implications, including anxiety and depression, and reduced quality of life. Bone health is severely compromised by long-term high cortisol levels, leading to osteoporosis. Cortisol affects bone metabolism by inhibiting osteoblast activity and promoting osteoclast activity, leading to bone resorption. This imbalance results in decreased bone density and increased fracture risk. High cortisol levels also interfere with calcium absorption and vitamin D metabolism, exacerbating bone loss. Over time, these effects lead to significant skeletal fragility and increased fracture risk, particularly in the elderly, impacting mobility and independence. Reproductive health is adversely affected by high cortisol levels, with significant implications for both men and women. In women, chronic elevation can lead to menstrual irregularities, reduced fertility, and pregnancy complications. Cortisol disrupts the hypothalamic-pituitary-gonadal axis, altering reproductive hormone secretion, such as estrogen and progesterone. In men, high cortisol levels can decrease testosterone production, leading to reduced libido, erectile dysfunction, and infertility. These issues can profoundly affect quality of life and psychological well-being, impacting personal relationships and contributing to stress and anxiety. The gastrointestinal system is another area impacted by long-term high cortisol levels, with potential consequences for digestive health. Cortisol affects gut motility and permeability, leading to conditions like irritable bowel syndrome (IBS) and increased intestinal permeability, or “leaky gut” syndrome. This results in digestive discomfort, nutrient malabsorption, and increased susceptibility to gastrointestinal infections. Chronic high cortisol can also alter gut microbiota, leading to dysbiosis, linked to inflammatory bowel disease and metabolic disorders. These effects underscore the importance of maintaining cortisol balance to prevent long-term health complications, including conditions like Cushing’s syndrome, characterized by prolonged exposure to high cortisol levels.
In what ways can mental health be affected?
Elevated cortisol levels, the primary stress hormone, can significantly affect mental health, leading to conditions such as anxiety and depression. Chronic stress results in sustained high cortisol, which disrupts neurotransmitter regulation, particularly serotonin and dopamine. This disruption is critical as these neurotransmitters are essential for mood stabilization. The imbalance can manifest as persistent feelings of sadness and anxiety, contributing to mental fatigue. Additionally, high cortisol levels can impair cognitive functions, such as memory and concentration, exacerbating mental health issues and potentially leading to insomnia. The interplay between cortisol and mental health is complex, with stress-induced cortisol release potentially leading to more severe conditions like Cushing’s syndrome. This syndrome is characterized by excessive cortisol production, which can cause significant weight gain and elevated blood pressure, further impacting mental health. The physiological changes associated with Cushing’s syndrome can exacerbate anxiety and depression, creating a cycle that is challenging to break. Moreover, the adrenal glands, responsible for cortisol production, can become overactive, further complicating mental health outcomes. High cortisol levels can also lead to cognitive impairments, affecting memory and executive function. Cortisol can interfere with synaptic plasticity, essential for learning and memory, leading to difficulties with attention and problem-solving. These cognitive challenges can worsen mental health disorders by affecting an individual’s ability to cope with stressors effectively. Furthermore, the chronic stress associated with elevated cortisol can result in adrenal fatigue, characterized by emotional exhaustion and a reduced sense of personal accomplishment, further impacting mental health. The relationship between elevated cortisol and stress-related disorders such as PTSD is significant. Individuals with PTSD often exhibit dysregulated cortisol patterns, exacerbating symptoms like intrusive memories and emotional numbing. The neurobiological changes induced by cortisol, such as altered amygdala function, contribute to the persistence of PTSD symptoms. Chronic stress and elevated cortisol can also lead to comorbid conditions like anxiety and depression, necessitating comprehensive treatment approaches to address the complex interplay of mental health challenges.
Effective Management and Treatment Strategies
Effective management of elevated cortisol levels involves addressing both physiological and psychological aspects of stress. One primary strategy is incorporating regular physical activity, which reduces cortisol levels and enhances stress resilience. Aerobic exercises, such as running and swimming, help normalize cortisol rhythms and improve mood. Mind-body practices like yoga can promote relaxation, reduce stress, and lower blood pressure. Exercise also counters weight gain associated with high cortisol, improving overall health. Nutritional interventions are crucial in managing cortisol levels. A diet rich in whole foods supports adrenal health and regulates cortisol production. Nutrients like omega-3 fatty acids and magnesium modulate cortisol levels and improve stress resilience. Reducing caffeine and sugar intake prevents cortisol spikes, promoting hormonal balance. Adequate hydration is essential, as dehydration can trigger cortisol release. Dietary supplements, such as adaptogens like ashwagandha, may support stress management by enhancing the body’s ability to cope with stressors. Cognitive-behavioral therapy (CBT) is effective for managing high cortisol levels. CBT focuses on altering negative thought patterns contributing to stress and anxiety. Addressing these psychological triggers helps develop healthier coping mechanisms, improving emotional regulation. Mindfulness-based interventions, such as mindfulness-based stress reduction (MBSR), enhance self-awareness, reduce cortisol levels, and promote relaxation. These therapeutic approaches, combined with lifestyle changes, provide a holistic framework for managing elevated cortisol levels. In severe cases, pharmacological interventions may be necessary. Medications like SSRIs manage anxiety and depression exacerbated by high cortisol levels. Some medications target cortisol production directly, reducing levels and alleviating symptoms. Pharmacological treatments should complement lifestyle, nutritional, and psychological interventions for optimal outcomes. A comprehensive approach ensures effective management of stress, hormone regulation, and associated mental health conditions.
What lifestyle modifications can help reduce cortisol?
Implementing lifestyle modifications is essential for reducing cortisol levels and mitigating the effects of stress. Regular physical activity is one of the most effective modifications. Exercise decreases cortisol levels and improves stress resilience. Activities like aerobic exercises, strength training, and yoga regulate cortisol production and enhance mood. Consistent exercise promotes hormonal balance, reducing the risk of stress-related health issues like weight gain and high blood pressure. Physical activity also releases endorphins, natural mood elevators that counteract cortisol effects. Sleep hygiene is critical for reducing cortisol levels. Quality sleep maintains healthy cortisol rhythms. Disrupted sleep patterns elevate cortisol, impairing cognitive function and emotional regulation. A consistent sleep schedule and a relaxing bedtime routine improve sleep quality, reducing cortisol production. Limiting screen time before bed and avoiding caffeine enhances sleep hygiene and cortisol regulation. Relaxation techniques like progressive muscle relaxation promote restful sleep, reducing nighttime cortisol levels and preventing insomnia. Stress management techniques are vital for lowering cortisol levels. Mindfulness practices like meditation and deep breathing reduce stress and cortisol production. These techniques promote relaxation and enhance the body’s ability to cope with stressors. Engaging in fulfilling activities like hobbies and socializing improves emotional well-being, decreasing cortisol levels. Establishing a work-life balance and setting boundaries prevent burnout, maintaining healthy cortisol levels. Gratitude and positive affirmations shift focus from stressors, supporting cortisol reduction. Nutritional strategies are essential in managing cortisol through lifestyle modifications. A balanced diet rich in whole foods supports adrenal health and regulates cortisol production. Nutrients like omega-3 fatty acids and vitamin C modulate cortisol levels, improving stress resilience. Reducing caffeine and sugar intake prevents cortisol spikes, promoting hormonal balance. Adaptogenic herbs like ashwagandha support stress management by enhancing the body’s ability to cope with stressors. These dietary changes, combined with other lifestyle modifications, provide a comprehensive approach to reducing cortisol levels and improving overall health.
- Permanently Closed Gyms in Singapore: Complete 2016-2025 List & Why You Need to Choose Wisely - December 29, 2025
- Beyond the Comfort Zone: Embracing the Unknown in Fitness and Life - November 14, 2025
- Why Traditional Gyms Don’t Work (And What Does): The Anti-Gym Revolution - November 14, 2025
