Introduction to Ketogenic Diet and Hashimoto’s Disease
The ketogenic diet, an eminent low-carb, high-fat dietary approach, has been recognized for its potential benefits in weight loss and metabolic health. The diet induces a metabolic state known as ketosis, in which the body utilizes fats, rather than carbohydrates, as its primary energy source. Simultaneously, Hashimoto’s disease, an autoimmune disorder affecting the thyroid gland, leads to hypothyroidism, a condition characterized by an underactive thyroid. Recent research suggests a potential intersection between the ketogenic diet and Hashimoto’s disease, with the low-carb diet potentially offering benefits for those with the autoimmune condition. The ketogenic diet’s high-fat, low-carb nature may help reduce inflammation, a common characteristic of autoimmune disorders like Hashimoto’s disease. Additionally, the diet’s ability to induce ketosis may support thyroid health and metabolism, potentially beneficial for those with hypothyroidism. However, it’s crucial to note that the research in this area is still in its infancy, and further studies are required to fully comprehend the potential benefits and drawbacks.

What is a Ketogenic Diet?
The ketogenic diet, a nutrition plan centered around low-carb, high-fat intake, has gained significant attention due to its potential benefits in weight loss, diabetes management, and neurological disorders. The diet’s primary goal is to induce a state of ketosis in the body, where the body burns fats instead of carbohydrates for energy. This metabolic state occurs when the body breaks down dietary and stored fat into molecules called ketones, which it uses for fuel. The ketogenic diet is characterized by a high intake of fats, moderate intake of proteins, and a minimal intake of carbohydrates. In a typical ketogenic diet, approximately 70-75% of calories come from fats, 20-25% from proteins, and only 5-10% from carbohydrates. This macronutrient distribution contrasts sharply with the common Western diet, which is generally high in carbohydrates and low in fats. While the ketogenic diet offers potential health benefits, it’s not suitable for everyone. The diet’s restrictive nature can make it challenging to follow, and without proper planning, it may lead to nutrient deficiencies. Some individuals may also experience side effects such as the “keto flu,” characterized by symptoms such as fatigue, nausea, and dizziness. Therefore, it’s advisable to consult a healthcare professional before starting a ketogenic diet.
Understanding Hashimoto’s Disease
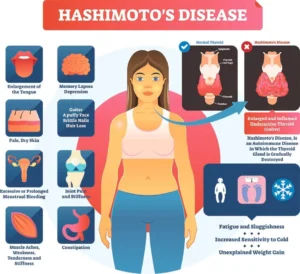
Hashimoto’s disease, also known as Hashimoto’s thyroiditis, is an autoimmune disorder that affects the thyroid gland. The thyroid gland, a small, butterfly-shaped gland located at the front of the neck, plays a crucial role in endocrinology, producing hormones that regulate the body’s metabolism, including heart rate, body temperature, and energy production. In Hashimoto’s disease, the immune system mistakenly attacks the thyroid gland, leading to inflammation and damage. This autoimmune response results in a gradual decrease in thyroid function, leading to hypothyroidism. Symptoms of Hashimoto’s disease can vary widely but may include fatigue, weight gain, sensitivity to cold, dry skin, and depression. The exact cause of Hashimoto’s disease remains unknown, but it’s thought to involve a combination of genetic and environmental factors. The disease is more common in women than in men and is most often diagnosed in middle-aged adults. Treatment typically involves hormone replacement therapy to restore normal thyroid function. While there’s currently no cure for Hashimoto’s disease, management strategies can help to alleviate symptoms and improve quality of life. These may include medication, lifestyle changes, and in some cases, dietary modifications such as a gluten-free or anti-inflammatory diet. It’s important to work closely with a healthcare provider to develop a personalized treatment plan.
What Causes Hashimoto’s?
Hashimoto’s disease, an autoimmune disorder, primarily targets the thyroid gland, leading to hypothyroidism. This autoimmune response is often triggered by a combination of genetic and environmental factors. Genetic predisposition is significant in Hashimoto’s development, with those having a family history of Hashimoto’s or other autoimmune disorders being more susceptible. Environmental factors, including exposure to radiation, certain chemicals, and specific medications, can increase the risk of developing this condition. In the field of endocrinology, Hashimoto’s is often associated with dietary factors. High intake of iodine and gluten can exacerbate Hashimoto’s, triggering an autoimmune response in genetically susceptible individuals. However, the relationship between diet and Hashimoto’s is complex. A gluten-free diet, for instance, may not always relieve symptoms, indicating the need for further research to clarify these relationships and develop dietary guidelines for individuals with Hashimoto’s.
Signs and Symptoms of Hashimoto’s
Hashimoto’s disease, a common cause of hypothyroidism, presents a wide range of signs and symptoms. Early symptoms often include fatigue, weight gain, cold intolerance, and joint and muscle pain, all resulting from a decline in thyroid function. As Hashimoto’s progresses, symptoms often become more pronounced, with individuals experiencing depression, memory lapses, and decreased concentration. Physical symptoms of Hashimoto’s can include hair loss, slow heart rate, and heavy or irregular menstrual periods. A common physical sign is a goiter, a swelling in the front of the neck, which occurs as the thyroid gland enlarges in response to the autoimmune attack. In severe cases, untreated Hashimoto’s can lead to a condition known as myxedema, characterized by extreme fatigue, cold intolerance, mental impairment, and other severe symptoms, highlighting the importance of individualized treatment approaches.
How Does a Ketogenic Diet Work?
The ketogenic diet, a high-fat, low-carb dietary approach, induces a metabolic state known as ketosis. By drastically reducing carbohydrate intake and increasing fat intake, the body shifts from using glucose as its primary energy source to using ketone bodies, altering the body’s energy metabolism. This metabolic shift is similar to the metabolic state of fasting, promoting weight loss and offering potential benefits for individuals with conditions such as diabetes or metabolic syndrome. The ketogenic diet also affects hormone regulation, particularly insulin. Insulin, a hormone that regulates blood sugar levels, plays a key role in the metabolism of carbohydrates and fats. By reducing carbohydrate intake, the ketogenic diet can help regulate insulin levels, potentially benefiting individuals with conditions such as diabetes or metabolic syndrome.
Principles of the Ketogenic Diet
The ketogenic diet is designed to induce ketosis through a drastic reduction in carbohydrate intake. This typically involves consuming less than 50 grams of carbohydrates per day. The majority of calories in the diet come from fats, with a moderate amount from proteins. The ketogenic diet emphasizes the consumption of foods high in healthy fats, such as avocados, nuts, seeds, and olive oil, and proteins from sources such as meat, fish, and eggs. Processed foods and sugars, high in carbohydrates, are generally avoided on the ketogenic diet. Instead, the diet encourages the consumption of whole, unprocessed foods, which can provide a range of nutrients and help to promote overall health. Regular physical activity is another important aspect of the ketogenic diet, helping to promote ketosis and enhance the benefits of the diet.
Foods to Include and Avoid in a Keto Diet
The ketogenic diet, a low-carb, high-fat nutritional approach, focuses on inducing the body into a state of ketosis. Ketosis is a metabolic state where the body burns fat as its primary energy source instead of carbohydrates. To achieve ketosis, it’s essential to include protein-rich foods like meats, fish, and eggs in the diet. These foods offer essential amino acids, vital for muscle development and repair, and contribute to weight loss due to their high satiety value. In addition, foods high in healthy fats such as avocados, nuts, and seeds play a vital role in a ketogenic diet. They provide the necessary fats that the body converts into ketones for energy, promoting ketosis. Low-carb vegetables such as spinach, broccoli, and cauliflower are also included for their rich nutritional content and minimal impact on blood sugar levels. Conversely, high-carb and sugary foods like bread, pasta, rice, beans, potatoes, and most fruits should be avoided in a ketogenic diet. These foods can disrupt ketosis, hindering the body’s ability to burn fat effectively. Processed foods and unhealthy fats, often laden with gluten, are also excluded due to their potential contribution to inflammation and other health issues.
How Does the Keto Diet Affect Thyroid Health?
The thyroid gland, an essential endocrinology component, is vital for metabolism, growth, and development. The ketogenic diet’s impact on thyroid health is a subject of continuous research. Some studies suggest that the low-carb diet can improve thyroid function in individuals with hypothyroidism, an underactive thyroid condition. The ketogenic diet’s anti-inflammatory properties may help reduce inflammation often associated with hypothyroidism. This, coupled with the diet’s potential to improve metabolic function, could contribute to better thyroid health. Moreover, the diet’s emphasis on nutrient-dense, gluten-free foods could potentially address nutrient deficiencies often seen in individuals with thyroid issues. However, other studies suggest that a ketogenic diet might suppress thyroid function by decreasing thyroid-stimulating hormone (TSH) levels, a crucial hormone for thyroid function. This suppression could potentially exacerbate thyroid issues, particularly in individuals with pre-existing thyroid conditions.
Intersecting Ketogenic Diet and Hashimoto’s
Hashimoto’s disease is an autoimmune condition where the immune system mistakenly attacks the thyroid gland. This attack leads to chronic inflammation and can potentially result in hypothyroidism. The ketogenic diet’s intersection with Hashimoto’s disease is multifaceted. The ketogenic diet’s anti-inflammatory properties could potentially help manage the inflammation associated with Hashimoto’s disease. By reducing inflammation, the diet could potentially minimize damage to the thyroid gland, promoting better thyroid function. Furthermore, the diet’s potential to improve metabolic function could be beneficial for individuals with Hashimoto’s disease, who often struggle with metabolic issues due to impaired thyroid function. However, the ketogenic diet’s potential to suppress thyroid function could be problematic for individuals with Hashimoto’s disease. As previously mentioned, the diet could potentially lower thyroid-stimulating hormone (TSH) levels, which could further impair thyroid function in individuals with Hashimoto’s disease.
Impact of Keto Diet on Hashimoto’s Symptoms
The ketogenic diet’s impact on Hashimoto’s symptoms can vary greatly among individuals. Some individuals have reported significant improvements in symptoms such as fatigue, weight gain, and brain fog while following the diet. These improvements could be attributed to the diet’s potential to improve metabolic function and reduce inflammation. However, other individuals have reported a worsening of symptoms or no change at all while following the diet. This variation in experiences could be due to the diet’s potential to suppress thyroid function, or it could be due to individual variations in how the body responds to the diet. Therefore, while the ketogenic diet could potentially help manage Hashimoto’s symptoms, its impact can vary greatly among individuals. It is not a cure-all and should not be used as the sole treatment for Hashimoto’s disease. Instead, it should be used as part of a comprehensive treatment plan, ideally under the supervision of a healthcare professional.
Scientific Studies and Evidence
Scientific research in the field of endocrinology has provided substantial evidence on the impact of the ketogenic diet on inducing ketosis for effective weight loss. Studies published in nutritional journals have demonstrated that a low-carb, high-fat diet can lead to significant weight loss and improvements in various health markers. In a study published in The Journal of Nutrition and Metabolism, the ketogenic diet was found to have a profound effect on weight loss and metabolic efficiency. Participants following a ketogenic diet experienced a state of ketosis, where the body burns fat for fuel instead of carbohydrates. This led to significant weight loss and improvements in blood lipid profiles. Furthermore, several studies have indicated the potential benefits of a ketogenic diet for individuals with autoimmune thyroid disorders. A gluten-free, low-carb diet has been linked to reductions in thyroid antibodies in individuals with autoimmune thyroid disease. This suggests that the ketogenic diet may have anti-inflammatory properties that can help manage autoimmune conditions.
Case Studies and Real-Life Experiences
Real-life experiences and case studies provide valuable insights into the practical implications of the ketogenic diet. For instance, a case study involving a woman with hypothyroidism and weight loss struggles showed significant improvements after adopting a ketogenic diet. After following a low-carb, gluten-free diet, she experienced a reduction in hypothyroidism symptoms and significant weight loss. This case study underscores the potential benefits of a ketogenic diet for weight loss and managing thyroid health. Another compelling case study involves a man with an autoimmune condition. His experience on a ketogenic diet resulted in significant weight loss and a decrease in inflammation, indicating the diet’s potential anti-inflammatory properties.
Precactions and Considerations
While the ketogenic diet offers potential benefits for weight loss and health improvement, it’s essential to approach it with caution. Before embarking on a ketogenic diet, it’s crucial to consult with a healthcare professional or a nutrition expert. They can provide personalized advice based on your health status and nutritional needs. The ketogenic diet’s high fat content can lead to elevated cholesterol levels and an increased risk of heart disease. Therefore, it’s crucial to focus on consuming healthy fats, such as avocados, nuts, seeds, and olive oil, rather than unhealthy fats like processed meats and fried foods. The ketogenic diet can also lead to nutrient deficiencies, particularly in vitamins and minerals found in fruits and grains, which are limited on the diet. To combat this, it’s recommended to consume a variety of nutrient-dense, low-carb vegetables and to consider taking a multivitamin supplement.
Possible Risks and Side Effects of the Keto Diet
The ketogenic diet, while beneficial for many, can also lead to several side effects and health risks. One of the most common side effects is the “keto flu,” a collection of symptoms including nausea, fatigue, headaches, and irritability that can occur as your body adapts to the diet. In addition to the keto flu, some individuals may experience constipation due to the reduced intake of dietary fiber. Drinking plenty of water and consuming high-fiber, low-carb vegetables can help alleviate this issue. Long-term adherence to the ketogenic diet can also lead to potential health risks. These include liver disease due to the high fat intake, kidney stones due to increased uric acid levels, and nutrient deficiencies due to the restrictive nature of the diet. Therefore, it’s crucial to monitor your health closely while on the ketogenic diet and to seek professional guidance as needed.
How to Support Digestive Health on Keto
The ketogenic diet, a renowned low-carb diet, propels the body into a state of ketosis, resulting in fat being used as the primary energy source. This low-carb, high-fat diet can sometimes cause digestive discomfort due to a drastic shift in dietary habits. To support digestive health while maintaining ketosis, one strategy is to consume sufficient fiber. Despite the low-carb nature of the keto diet, there are high-fiber foods compatible with it, such as avocados, nuts, and non-starchy vegetables. Hydration, another critical aspect of the ketogenic diet, aids in digestion and can help prevent constipation, a common side effect of a low-carb diet. Probiotics, beneficial bacteria that support gut health, can also be beneficial. They can be found in foods like yogurt and sauerkraut or in supplement form. Lastly, consider digestive enzymes. These supplements can help your body break down the high amounts of fats consumed on a keto diet, aiding in nutrition absorption and promoting overall digestive health.
Important Nutrients and Supplements for Hashimoto’s
Hashimoto’s disease, an autoimmune disorder that can cause hypothyroidism, often requires a focus on specific nutrients and supplements for optimal health. Selenium is one such nutrient. It plays a crucial role in the conversion of thyroid hormone and can help reduce thyroid antibodies. Brazil nuts are a rich source of selenium, but it can also be taken as a supplement. Another important nutrient is Zinc. It is essential for thyroid hormone production and can help boost immune function. Zinc can be found in foods like oysters, beef, and pumpkin seeds or as a supplement. Vitamin D deficiency is common in individuals with Hashimoto’s. It plays a vital role in immune function and can help reduce thyroid antibodies. Sunlight is a great source of vitamin D, but it can also be obtained through supplements or foods like fatty fish and fortified dairy products. Lastly, consider Omega-3 fatty acids. They are known for their anti-inflammatory properties and can help support thyroid function. Omega-3s can be found in fatty fish, flaxseeds, and chia seeds, or taken as a supplement.
Concluding Thoughts: Is Keto Suitable for Hashimoto’s?
The ketogenic diet’s suitability for Hashimoto’s disease is a topic of ongoing debate within the medical community. On one hand, the ketogenic diet can help reduce inflammation, a key factor in autoimmune diseases like Hashimoto’s. The diet’s high fat content can also support hormone production, including thyroid hormones. On the other hand, the ketogenic diet’s restrictive nature can make it challenging to obtain all necessary nutrients. This is particularly concerning for individuals with Hashimoto’s, who often require specific nutrients for optimal health. Moreover, the diet’s potential impact on gut health could exacerbate autoimmune symptoms. Therefore, while the ketogenic diet may offer benefits for some individuals with Hashimoto’s, it is not suitable for everyone. It’s always best to consult a healthcare professional before starting a new diet, particularly if you have an existing health condition.
Weighing the Pros and Cons
When considering the ketogenic diet for Hashimoto’s, it’s important to weigh the pros and cons. On the pro side, the diet can help reduce inflammation and support hormone production. It can also lead to weight loss, which can be beneficial for individuals with hypothyroidism, a common symptom of Hashimoto’s. On the con side, the diet’s restrictive nature can make it challenging to obtain all necessary nutrients. This is particularly concerning for individuals with Hashimoto’s, who often require specific nutrients for optimal health. Moreover, the potential impact on gut health could exacerbate autoimmune symptoms. Finally, it’s important to consider the diet’s sustainability. The ketogenic diet requires a significant commitment and may not be sustainable for everyone in the long term. As always, it’s best to consult a healthcare professional before starting a new diet, particularly if you have an existing health condition.
Personalizing the Diet for Your Needs
Personalizing a diet involves understanding the nuances of individual health and nutritional needs. For instance, a person with hypothyroidism, an autoimmune disorder, may require a diet that supports thyroid function and reduces inflammation. In such cases, an anti-inflammatory diet, which is low in processed foods and high in fruits, vegetables, and healthy fats, may be recommended. Moreover, the concept of ketosis has gained traction in nutrition and weight loss circles. Achieving ketosis, a metabolic state where the body burns fat for energy instead of carbohydrates, requires a low-carb diet. This diet can be personalized based on individual needs and preferences. Gluten-free diets are another aspect of personalized nutrition. This diet is essential for individuals with celiac disease, an autoimmune disorder, but may also provide benefits for others. Personalizing a gluten-free diet involves ensuring that all sources of gluten are eliminated while still meeting nutritional needs.
Consulting Healthcare Professionals
When personalizing a diet, consulting healthcare professionals is crucial. These professionals provide invaluable expertise in various fields, including nutrition, endocrinology, and dietetics. For instance, an endocrinologist can provide crucial insights into managing conditions like hypothyroidism or other thyroid-related issues. Dietitians and nutritionists are experts in the field of nutrition. They can provide guidance on a variety of diets, from low-carb diets for weight loss or achieving ketosis, to gluten-free diets for managing autoimmune disorders. They can also provide advice on anti-inflammatory diets, which can be beneficial for individuals with autoimmune disorders. Furthermore, these professionals can offer ongoing support and monitoring. This can involve tracking progress, making necessary adjustments to the diet, and providing support and motivation. This professional guidance can be instrumental in achieving health goals and ensuring the diet is both nutritionally adequate and sustainable.
- Permanently Closed Gyms in Singapore: Complete 2016-2025 List & Why You Need to Choose Wisely - December 29, 2025
- Beyond the Comfort Zone: Embracing the Unknown in Fitness and Life - November 14, 2025
- Why Traditional Gyms Don’t Work (And What Does): The Anti-Gym Revolution - November 14, 2025
